This is a sample of what a typical traumatic lecture page looks like. We've made it accessible so that you can get an idea of whether or not this format works for you. Take some time to read through the material. Videos help explain complex concepts; remember to turn your audio on.
Respiratory Distress & Arrest
This page focuses on understanding the pathophysiology, assessment, and treatment of traumatic injuries to the chest and respiratory system. The material on this page is summarized for field use in the Trauma section of the Wilderness Medicine Handbook.
Contents
Contents
Normal Anatomy & Physiology
|
Normal Anatomy & Physiology
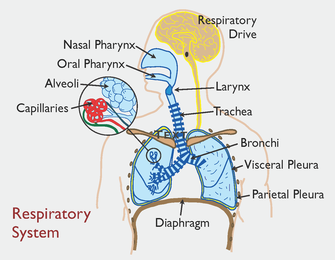
The function of the respiratory system is to supply the blood with oxygen and remove carbon dioxide (carbon dioxide is acidic and its removal helps to maintain blood pH). Air enters and leaves the lungs via a set of air chambers (nasal and/or oral pharynx) and tubes (trachea, and bronchi). The lungs are a combination of air tubes (bronchi) and blood vessels that interface at tiny air sacks (alveoli) where the gas exchange takes place. The air tubes, blood vessels, and alveoli are held together by elastic connective tissue and surrounded by a resilient membrane called the visceral pleura. A second membrane, the parietal pleura, lines the interior of the chest cavity and is attached to the intercostal muscles and diaphragm. The parietal pleura is separated from the visceral pleura by a lubricating fluid. During respiration, the two are held together by the surface tension of the fluid. |
Breathing
Rising carbon dioxide levels stimulate chemoreceptors in the brain stem that signal the diaphragm and intercostal muscles to contract. Once triggered, the chest and lungs expand. As the intrathoracic space enlarges a negative pressure begins to build internally; and, in a process similar to that of expanding bellows, air is pulled into the lungs through the mouth or nose. The air passes through a series of smaller and smaller tubes (trachea, bronchi, bronchioles) until it fills microscopic air sacs (alveoli) and the pressure is equalized. The alveoli are enveloped by capillary beds and it is through the thin walls of the alveoli and the adjacent capillaries that the gas exchange takes place.
While inspiration is an active process, expiration is passive. During expiration the muscles relax, intrathoracic pressure increases, and air is expelled. Normal respirations are smooth, easy and quiet.
Rising carbon dioxide levels stimulate chemoreceptors in the brain stem that signal the diaphragm and intercostal muscles to contract. Once triggered, the chest and lungs expand. As the intrathoracic space enlarges a negative pressure begins to build internally; and, in a process similar to that of expanding bellows, air is pulled into the lungs through the mouth or nose. The air passes through a series of smaller and smaller tubes (trachea, bronchi, bronchioles) until it fills microscopic air sacs (alveoli) and the pressure is equalized. The alveoli are enveloped by capillary beds and it is through the thin walls of the alveoli and the adjacent capillaries that the gas exchange takes place.
While inspiration is an active process, expiration is passive. During expiration the muscles relax, intrathoracic pressure increases, and air is expelled. Normal respirations are smooth, easy and quiet.