This is a sample of what a typical medical lecture page looks like. We've made it accessible so that you can get an idea of whether or not this format works for you. Videos help explain complex concepts; remember to turn your audio on.
Circulatory System Problems
This page focuses on understanding the pathophysiology, assessment, and
treatment of medical circulatory system problems. The material on this
page is summarized for field use in the Heart Attack & Angina, Congestive Heart Failure, Cardiogenic Shock, Aortic Aneurysm & Dissection, and Stroke (CVA or TIA) sections of the Wilderness Medicine Handbook.
Contents
Contents
Atherosclerosis
Pathophysiology
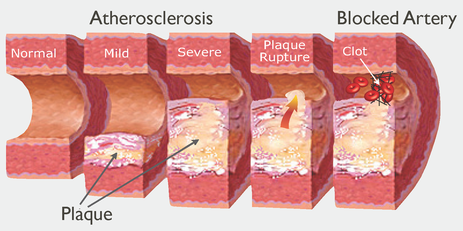
Over time arteries that were once healthy may become obstructed by plaque as fats—cholesterol and triglycerides—are deposited within their walls. The deposits lead to inflammation and scarring, and the normal elastic nature of the arterial walls is eventually lost. As the plaque thickens, the blood flow at the site of the constriction is reduced, slowing the delivery of blood and nutrients to the downstream tissue and increasing blood pressure. The process is so gradual that the body accepts the existence of arterial plaque as a normal development. If the plaque ruptures, the body senses an “abnormal” disturbance in the arterial wall and initiates the clotting process at the site of the disturbance.
Over time arteries that were once healthy may become obstructed by plaque as fats—cholesterol and triglycerides—are deposited within their walls. The deposits lead to inflammation and scarring, and the normal elastic nature of the arterial walls is eventually lost. As the plaque thickens, the blood flow at the site of the constriction is reduced, slowing the delivery of blood and nutrients to the downstream tissue and increasing blood pressure. The process is so gradual that the body accepts the existence of arterial plaque as a normal development. If the plaque ruptures, the body senses an “abnormal” disturbance in the arterial wall and initiates the clotting process at the site of the disturbance.
Once the clot is fixed in place it cuts off perfusion to the tissue serviced by the artery. If the tissue is not adequately supplied by collateral circulation, it will die. Risk factors for atherosclerosis include: obesity, a high-fat diet, high blood pressure, smoking, no or low exercise, chronic stress, and a family history of atherosclerosis.
Prevention
Prevention
- Eliminate the associated risk factors by eating a healthy diet; engage in a daily aerobic exercise program, don’t smoke, treat high blood pressure, and eliminate stress.
- Minerals that help strengthen the circulatory system include: copper, chromium, calcium, magnesium, and selenium.
- Additional supplements include vitamins E and C, lecithin, and coenzyme Q. Vitamin D is also important for cardiovascular health and optimum levels are best achieved through diet and daily sun exposure.
- Helpful herbs include raw garlic and licorice.
- Medications are available to decrease serum cholesterol and control high blood pressure.
Angina & Heart Attacks
Heart Attack Pathophysiology
Developing atherosclerosis, plaque rupture, and subsequent clotting of a coronary artery is the most common cause of heart attacks. Signs and symptoms commonly appear immediately and are due to a lack of oxygen in the affected tissue. Cardiac arrest evolves along a continuum and is not predictable. Arrest is ultimately due to a change in the electrical impulses and conduction pattern (cardiac arrhythmia) in the specialized cardiac nerves that stimulate normal cardiac contractions. An injury to these nerves blocks the conduction pathway. The block prevents or delays the electrical impulses from reaching their destination and causes cardiac arrest. The potential for arrest from a heart attack is directly related to the type, location, and size of the compromised tissue and therefore unpredictable. If the blocked artery services the specialized conduction cells that coordinate the pumping action of the heart, arrest occurs within seconds or minutes. If the blocked artery services the heart’s contractile fibers rather than its specialized conduction cells, the pumping action of the heart may be compromised. A reduction in the heart’s ability to pump blood efficiently may cause a back pressure in the pulmonary vessels and force fluid into the alveoli causing respiratory distress, fatigue, swelling in the hands and feet, indigestion and loss of appetite. Complete pump failure and arrest may develop if a significant amount of heart muscle has been injured and the heart cannot continue to meet the body’s demands for nutrients. The longer arrest is delayed the more likely the patient will survive without immediate hospital treatment. Patients who survive heart attacks are usually tired and “feel sick” with slightly elevated pulse and respiratory rates. Recovery often takes months or years. Subsequent heart attacks are possible.
Developing atherosclerosis, plaque rupture, and subsequent clotting of a coronary artery is the most common cause of heart attacks. Signs and symptoms commonly appear immediately and are due to a lack of oxygen in the affected tissue. Cardiac arrest evolves along a continuum and is not predictable. Arrest is ultimately due to a change in the electrical impulses and conduction pattern (cardiac arrhythmia) in the specialized cardiac nerves that stimulate normal cardiac contractions. An injury to these nerves blocks the conduction pathway. The block prevents or delays the electrical impulses from reaching their destination and causes cardiac arrest. The potential for arrest from a heart attack is directly related to the type, location, and size of the compromised tissue and therefore unpredictable. If the blocked artery services the specialized conduction cells that coordinate the pumping action of the heart, arrest occurs within seconds or minutes. If the blocked artery services the heart’s contractile fibers rather than its specialized conduction cells, the pumping action of the heart may be compromised. A reduction in the heart’s ability to pump blood efficiently may cause a back pressure in the pulmonary vessels and force fluid into the alveoli causing respiratory distress, fatigue, swelling in the hands and feet, indigestion and loss of appetite. Complete pump failure and arrest may develop if a significant amount of heart muscle has been injured and the heart cannot continue to meet the body’s demands for nutrients. The longer arrest is delayed the more likely the patient will survive without immediate hospital treatment. Patients who survive heart attacks are usually tired and “feel sick” with slightly elevated pulse and respiratory rates. Recovery often takes months or years. Subsequent heart attacks are possible.
|
|
|
Angina Pathophysiology
Atherosclerosis reduces the amount of oxygen available to the heart by effectively shrinking the size of the arteries with plaque deposits. Exercise and stress can increase the heart’s need for oxygen beyond the delivery capacity of the restricted arteries. The resulting hypoxia causes heart pain or angina. Once the exercise or stress is removed, the oxygen requirements of the patient’s heart will return to normal levels and the chest pain will subside, usually within 20 minutes.
Atherosclerosis reduces the amount of oxygen available to the heart by effectively shrinking the size of the arteries with plaque deposits. Exercise and stress can increase the heart’s need for oxygen beyond the delivery capacity of the restricted arteries. The resulting hypoxia causes heart pain or angina. Once the exercise or stress is removed, the oxygen requirements of the patient’s heart will return to normal levels and the chest pain will subside, usually within 20 minutes.
Heart Attack S/Sx
- The classic signs and symptoms of a heart attack are non-traumatic chest pain or pressure accompanied by shortness of breath and diaphoresis (pale, sweating skin). Initially it is difficult to tell the difference between angina and a heart attack.
- Patient complains of non-traumatic chest pain. The pain may mimic indigestion and is typically described as pressure or squeezing. The pain may radiate to the patient’s neck or arms (classically the left arm but can be either arm or both).
- Rule out musculoskeletal mechanisms.
- Shortness of breath is common as are sweating and pale skin.
- Fatigue and weakness are present.
- Many patients deny the possibility of a heart attack.
- Cardiac arrest evolves along a continuum and is not predictable. From the onset of chest pain, arrest may occur within seconds to minutes if the heart’s conduction cells are affected, or within hours.
- If a large area of cardiac muscle is damaged (typically due to a heart attack), pump performance will decrease. Arrest is unlikely if a very small area of cardiac muscle is affected and pump performance remains relatively unaffected.
- Rising pulse and respiratory rates, decreasing mental status, and a falling blood pressure are the hallmarks of cardiogenic shock.
- Increased respiratory distress and developing edema (fluid) in the lungs, hands, and feet indicate congestive heart failure. It occurs when the left ventricle is damaged from a heart attack and can no longer effectively pump blood to the body. The blood backs up in the pulmonary vein increasing pressure in the pulmonary capillaries and forcing plasma into the alveoli. Fatigue, weakness, fainting accompanied by weight gain are common, as are loss of appetite, indigestion, nausea, and vomiting.
Heart Attack Treatment
- Because it is difficult to distinguish between angina and a heart attack in the initial stages, field treatment is identical.
- If respiratory distress is present, allow patient to sit or support them in a sitting position. Provide rest, reassurance, and oxygen.
- Begin a Level 1 Evacuation with ALS for all patients with a suspected heart attack.
- Administer 160-325 mg of chewable baby aspirin with the onset of chest pain. The aspirin acts as an anticoagulant and may help minimize cardiac damage, especially in patients with partial blockages.
- Administer nitroglycerin in awake patients with a current prescription. Adult dose is one tablet (.4 mg) dissolved under the patient’s tongue OR .4 mg delivered as a metered spray. The dose may be repeated every 5 minutes for three doses. Nitroglycerin will cause a tingling or burning sensation if it is active. Headaches are common following the administration of nitroglycerin and rarely last longer than 20 minutes. Chest pain should resolve within a few minutes if due to angina. If patient’s BP < 100 systolic, patient reports dizziness, or faints, DO NOT give additional nitroglycerin. DO NOT give nitroglycerin if patient is currently taking meds for erectile dysfunction (Viagra®, Cialis®, etc.).
- Begin CCR (chest compressions only) if the patient’s arrest is due to heart attack and rapid defibrillation—less than five minutes—and ALS intervention is possible. Compress hard and fast.
- Begin CPR (chest compressions and rescue breathing) if defibrillation and ALS intervention may be delayed greater than five minutes. Compress hard and fast. Ventilate until the patient’s chest begins to rise; do not overinflate. The ratio of compressions to ventilations is thirty compressions to two breaths. Use high flow supplemental oxygen if available. Be prepared for vomiting.
- Defibrillate if VF or pulseless VT have been confirmed regardless of core temperature (AED will advise shock).
- If resuscitation is successful, begin a Level 1 Evacuation to the nearest hospital.
- Consider stopping resuscitation efforts after 30 minutes of documented arrest.
- Support critical systems and begin a Level 1 Evacuation with ALS to a major hospital.
- Allow the patient to sit or support them in a sitting position. Provide rest, reassurance, and high liter flow oxygen.
- If the patient has a history of CHF and their own diuretic medication, allow them to continue taking it on schedule.
- If the patient has a prescription for nitroglycerin, they should take it.
- Begin a Level 1 Evacuation with ALS to a major hospital.
Stroke
Stroke Pathophysiology
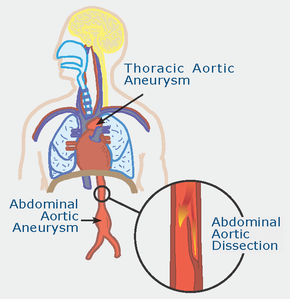
Most strokes are caused by embolotic clots breaking off from the carotid arteries and drifting into the cerebral vasculature or the rupture of a cerebral artery (cerebral aneurism). With an ischemic stroke (clot) the tissue serviced by the blocked artery loses perfusion and dies within a few minutes. Hemorrhagic strokes (bleeding) may lead to increased ICP. The signs and symptoms reflect the amount of brain damage. In extremely mild cases the patient has no noticeable loss of function and the stroke may go undetected. Serious cerebral blocks or aneurysms may be large enough to be instantly fatal. The loss of sensation and motor function in the patient is proportional to the severity and location of the stroke. Because the cerebrum is divided into two hemispheres by the corpus callosum (right and left brain) and each hemisphere is serviced by a separate arterial supply, tissue damage due to stroke is usually confined to a single side. Motor and sensory functions for the head and face are serviced by cranial nerves while the remainder of the body is serviced by spinal nerves. Because the spinal nerves cross in the brain stem, loss of sensation and motor function in the head and face reflect damage to the same side of the brain while a loss of function below the head reflects damage to the opposite side of the brain.
Most strokes are caused by embolotic clots breaking off from the carotid arteries and drifting into the cerebral vasculature or the rupture of a cerebral artery (cerebral aneurism). With an ischemic stroke (clot) the tissue serviced by the blocked artery loses perfusion and dies within a few minutes. Hemorrhagic strokes (bleeding) may lead to increased ICP. The signs and symptoms reflect the amount of brain damage. In extremely mild cases the patient has no noticeable loss of function and the stroke may go undetected. Serious cerebral blocks or aneurysms may be large enough to be instantly fatal. The loss of sensation and motor function in the patient is proportional to the severity and location of the stroke. Because the cerebrum is divided into two hemispheres by the corpus callosum (right and left brain) and each hemisphere is serviced by a separate arterial supply, tissue damage due to stroke is usually confined to a single side. Motor and sensory functions for the head and face are serviced by cranial nerves while the remainder of the body is serviced by spinal nerves. Because the spinal nerves cross in the brain stem, loss of sensation and motor function in the head and face reflect damage to the same side of the brain while a loss of function below the head reflects damage to the opposite side of the brain.
Stroke S/Sx
- History may indicate amnesia.
- S/Sx may disappear within 24 hours; medically, this is known as a Transient Ischemic Attack (TIA) and in a remote setting is treated as a stroke.
- Patients present with a loss of sensation and motor function involving a single hemisphere (same side face, opposite side body). Slurred speech & partial paralysis are common. Ask patient to smile and repeat a simple rhyme. If the smile is lopsided or their speech slurred, they have had a stroke. Compare their arm strength on both sides by asking them to hold both arms straight out in front of them at shoulder height and keep them there. If one arm drops lower than the other, they have had a stroke.
- Most awake patients are lethargic and tired immediately following a stroke.
- Some patients may present with a depressed level of consciousness. These patients generally have a poorer prognosis.
- Examine scene for fall; rule out traumatic problems as normal.
Stroke Treatment
- Administer oxygen if available.
- Sleep is a necessary part of the recovery process. A stroke patient should be permitted to sleep, closely monitored while sleeping, and awakened every few hours during the 24-hour period following the event.
- Begin a Level 1 Evacuation for all stroke patients to a major hospital; small strokes may be followed by more serious ones. IV thrombolytic medications are indicated ASAP and typically are best given within three hours but may be given up to 12 hours later if the stroke is due to a blocked blood vessel and there are no contraindications. Mechanical clot removal may be of benefit up to 12 hours after the initial insult. Surgery may be indicated if the stroke is due to a ruptured vessel. A CAT scan is required to distinguish between the various treatment options.
- Transport V, P, or U patients on their side.